Unlock the secrets to overcoming Posterior Tibial Tendon Dysfunction (PTTD) with our comprehensive guide. Learn about causes, symptoms, and effective treatments to restore your foot health and mobility today!

Introduction
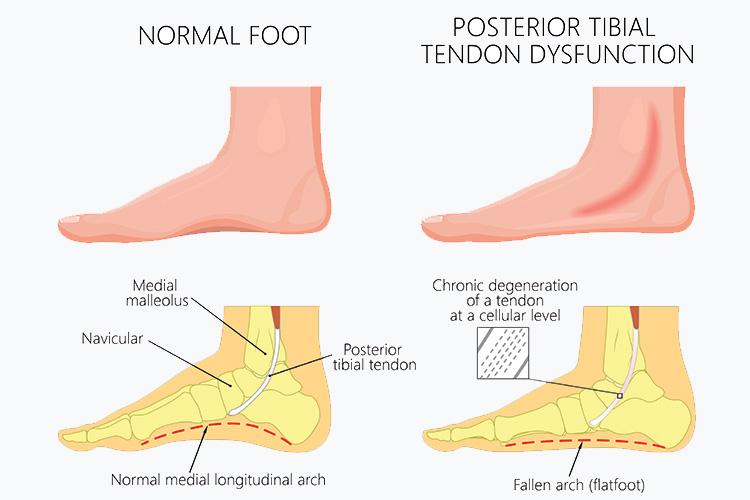
Posterior Tibial Tendon Dysfunction (PTTD) is a condition that affects the foot and ankle, leading to changes in the shape of the foot, pain, and in severe cases, disability. The posterior tibial tendon plays a crucial role in supporting the arch of your foot and helping you walk. Dysfunction in this tendon can cause the foot’s arch to collapse, leading to a condition commonly referred to as flatfoot. This article aims to shed light on Posterior Tibial Tendon Dysfunction, its causes, symptoms, and effective management strategies to help you maintain foot health and mobility.
Table of Contents
Overview of Posterior Tibial Tendon Dysfunction
PTTD is a condition that significantly impacts the structural integrity and functionality of the foot. The posterior tibial tendon, which is crucial for supporting the foot’s arch and enabling efficient movement, can deteriorate due to various factors. This deterioration leads to a progressive flattening of the foot, known as acquired adult flatfoot deformity, which can severely affect an individual’s ability to perform daily activities and maintain an active lifestyle.
Causes and Risk Factors of Posterior Tibial Tendon Dysfunction

Understanding the multifaceted causes and risk factors of PTTD is essential for both prevention and early intervention:
Overuse and Activity-Related Stress
Athletes, dancers, and individuals whose occupations require extended periods of standing or walking are at heightened risk due to repetitive stress on the tendon.
Injury and Trauma
Direct trauma to the posterior tibial tendon or ankle can initiate a cascade of events leading to dysfunction. This includes severe sprains that are not adequately treated or repetitive microtrauma that accumulates over time.
Biomechanical Factors
Individuals with an abnormal foot structure, such as flat feet or an overly pronated foot posture, may place additional stress on the posterior tibial tendon, predisposing it to dysfunction.
Systemic Conditions
Diseases that affect the body’s overall health and vascular supply, such as diabetes and hypertension, can compromise the tendon’s structural integrity and healing capacity. Inflammatory conditions like rheumatoid arthritis directly affect the tendon’s health by promoting inflammation and degenerative changes.
In-Depth Look at Symptoms
The progression of Posterior Tibial Tendon Dysfunction is often gradual, making early recognition of symptoms critical for effective management:
Progressive Pain and Swelling
Initially, pain might be intermittent, worsening with activity and improving with rest. As the condition advances, pain can become persistent, affecting daily activities.
Change in Foot Shape and Function
The gradual collapse of the arch leads to a visible flattening of the foot. This structural change can make it challenging to stand on tiptoes and may lead to an altered gait to compensate for the discomfort and loss of stability.
Secondary Symptoms
As the foot’s structure changes, secondary symptoms such as pain in the knees, hips, and lower back can develop due to the altered biomechanics of walking.

Diagnosis of Posterior Tibial Tendon Dysfunction
Early and accurate diagnosis of PTTD is crucial for effective treatment and to prevent further deterioration of the tendon and foot structure. The diagnostic process typically involves:
Physical Examination
A healthcare provider will examine the foot for signs of flatfoot deformity, swelling, and tenderness along the course of the posterior tibial tendon. They will also assess the flexibility, strength, and alignment of the foot and ankle.
Gait Analysis
Observing the patient’s walk can reveal the characteristic flatfoot gait and heel tilt associated with PTTD.
Imaging Tests
- X-rays are used to assess the alignment of the foot and look for changes in the shape of the foot that occur with PTTD.
- MRI (Magnetic Resonance Imaging) provides detailed images of soft tissues, including the posterior tibial tendon, to evaluate the extent of tendon damage or degeneration.
- Ultrasound may also be used to visualize the tendon’s condition and any tears or inflammation.
Treatment Options for Posterior Tibial Tendon Dysfunction
The treatment plan for PTTD is tailored to the individual’s specific stage of the condition and symptoms, aiming to relieve pain, restore function, and prevent progression.
Rest and Ice
Initial treatment often includes rest to reduce stress on the tendon and ice applications to decrease swelling and pain.
Orthotics
Custom-fitted orthotic devices can provide the necessary support to the arch, redistributing pressure away from the affected tendon and alleviating stress.
Bracing
For more significant tendon damage, a brace or walking boot may be necessary to stabilize the foot and ankle, allowing the tendon to rest and heal.
Physical Therapy
A targeted physical therapy program can strengthen the muscles around the foot and ankle, improve range of motion, and promote tendon healing. Specific exercises may also help correct any abnormal gait patterns.
Medications
NSAIDs, such as ibuprofen or naproxen, can be effective in reducing pain and inflammation during the acute phases of PTTD.
Surgery
If conservative treatments fail to provide relief or if the deformity progresses, surgical options may be considered. Surgical procedures can range from tendon repair or reconstruction to osteotomies (cutting and realigning bones) and arthrodesis (joint fusion) to correct alignment and restore function.
Prevention Strategies for PTTD
While it may not be possible to prevent PTTD entirely, especially in individuals with predisposing factors, the following strategies can minimize the risk and potentially slow the progression of the condition:
Maintain a Healthy Weight
Excess weight increases the load and stress on the posterior tibial tendon and foot structures. Achieving and maintaining a healthy weight through diet and exercise can reduce this strain.
Supportive Footwear
Shoes with proper arch support and cushioning can help distribute pressure evenly across the foot, reducing the load on the posterior tibial tendon. Avoid wearing high heels or shoes with inadequate support for extended periods.
Strengthening and Flexibility Exercises
Regular exercises that strengthen the muscles supporting the foot and ankle and improve flexibility can enhance foot stability and function. This includes exercises specifically targeting the posterior tibial tendon.
Activity Modification
Be mindful of activities that place excessive stress on the posterior tibial tendon. Alternating high-impact activities with low-impact exercises and incorporating rest periods can help manage stress on the tendon.
Frequently Asked Questions
Q: What is Posterior Tibial Tendon Dysfunction (PTTD)?
A: PTTD is a condition where the posterior tibial tendon, crucial for supporting the foot’s arch, deteriorates. This can lead to a flattening of the foot, known as acquired adult flatfoot deformity, affecting your ability to walk and perform daily activities.
Q: What causes PTTD?
A: Causes include overuse, injury, biomechanical factors, and systemic conditions like diabetes. Athletes, dancers, and people with flat feet are at higher risk.
Q: How do I know if I have PTTD?
A: Symptoms include progressive pain, swelling, changes in foot shape, and difficulty standing on tiptoes. If you notice these signs, consulting a healthcare provider is crucial for an accurate diagnosis.
Q: What are the treatment options for PTTD?
A: Treatment ranges from rest, ice, and orthotics to physical therapy and medications. In severe cases, surgery might be necessary to repair or reconstruct the tendon.
Q: Can PTTD be prevented?
A: While not entirely preventable, maintaining a healthy weight, wearing supportive footwear, and engaging in strengthening exercises can minimize risk and slow progression.
Conclusion
Posterior Tibial Tendon Dysfunction doesn’t have to dictate the terms of your mobility and life quality. With the right knowledge, early detection, and appropriate management strategies, you can navigate the challenges of PTTD and keep your feet healthy and functional. Remember, taking proactive steps towards foot health today can pave the way for a pain-free tomorrow. If you suspect PTTD symptoms, don’t hesitate to seek professional advice and tailor a treatment plan that suits your needs. Together, let’s step forward into a future where every step is pain-free and full of promise.