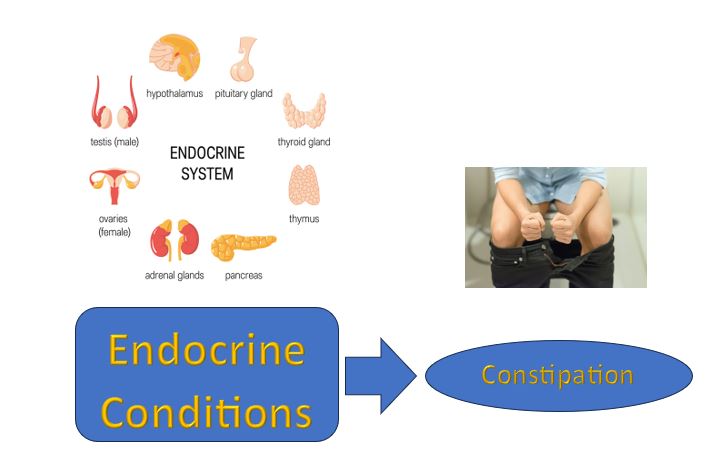
Constipation, a common gastrointestinal complaint affecting millions worldwide, often triggers a search for its underlying causes. Among the other factors implicated, endocrine health conditions frequently are found to be responsible.
While it’s undeniable that certain endocrine disorders can indeed contribute to constipation, attributing constipation complexation solely to these conditions oversimplifies a multifaceted issue.
Here We’ll See Thoroughly……
Constipation Complexity:
Constipation isn’t always a straightforward issue with a single cause. Instead, it’s a complex interplay of various factors that can disrupt regular bowel movements and lead to discomfort.

At its core, constipation involves difficulty passing stools or infrequent bowel movements.
While some cases may be attributed to temporary factors like changes in diet or dehydration, others may be more persistent and indicative of underlying issues.
- One of the primary contributors to constipation complexity is lifestyle.
- Poor dietary habits, such as low fiber intake, can slow down digestion and make stools harder to pass.
- Similarly, inadequate hydration and lack of physical activity can contribute to sluggish bowel movements.
- Medical conditions also play a significant role.
- Endocrine disorders like hypothyroidism can affect metabolism and digestion, leading to constipation.
- Neurological conditions, such as Parkinson’s disease, can disrupt the signals between the brain and the gut, impacting bowel function.
- Moreover, certain medications, including opioids and some antidepressants, are known to cause constipation as a side effect.
- Even psychological factors like stress and anxiety can influence gut motility and exacerbate constipation.
Understanding the complexity of constipation is crucial for effective management. Treatment often involves a holistic approach that addresses underlying causes while also focusing on lifestyle modifications.
The Role of Endocrine Health Conditions:
Endocrine health conditions can indeed contribute to constipation in some cases, although it’s essential to recognize that constipation can have multiple causes, including dietary factors, dehydration, lack of physical activity, and certain medications.
However, several endocrine disorders can affect bowel function and potentially lead to constipation.

Here are a few examples:
- Hypothyroidism:
- When the thyroid gland doesn’t produce enough thyroid hormone, it can slow down bodily functions, including digestion.
- This can lead to constipation as the digestive tract moves food through the intestines more slowly.
- Hyperparathyroidism:
- Overactivity of the parathyroid glands, which regulate calcium levels in the body, can lead to constipation as well as other gastrointestinal symptoms.
- Diabetes Mellitus:
- Diabetes can affect nerves throughout the body, including those that control the gastrointestinal tract.
- Diabetic neuropathy can slow down the movement of food through the intestines, leading to constipation.
- Hypopituitarism:
- This condition involves decreased function of the pituitary gland, which can lead to hormonal imbalances affecting various bodily functions, including digestion.
- Constipation can be one of the symptoms of hypopituitarism.
- Adrenal Insufficiency:
- Insufficient production of adrenal hormones, such as cortisol, can disrupt normal bowel function and contribute to constipation.
It’s important to note that constipation alone may not necessarily indicate an endocrine disorder, as it can also result from other factors mentioned earlier.
Other Causes of Constipation:
Constipation, a condition characterized by infrequent bowel movements or difficulty passing stools, can be caused by a variety of factors beyond endocrine disorders. While conditions such as hypothyroidism and diabetes can indeed contribute to constipation, it’s essential to recognize that several other factors play a significant role in its development.

Understanding these additional causes is crucial for effectively managing and addressing constipation. Here are some common contributors beyond endocrine disorders:
- Dietary Factors:
- One of the most common causes of constipation is a diet low in fiber.
- Fiber adds bulk to stool and helps it move through the digestive tract more efficiently.
- Inadequate intake of fruits, vegetables, whole grains, and other fiber-rich foods can lead to constipation.
- Additionally, not drinking enough water can exacerbate the problem, as fiber needs water to work effectively.
- Lack of Physical Activity:
- Physical activity stimulates the muscles in the digestive tract, promoting bowel movements.
- A sedentary lifestyle can contribute to constipation by slowing down these muscle contractions.
- Regular exercise can help prevent and alleviate constipation by promoting healthy bowel function.
- Medications:
- Certain medications can have constipation as a side effect.
- These may include opioid pain medications, antacids containing calcium or aluminum, some antidepressants, and certain antispasmodic drugs.
- If you suspect that a medication you’re taking is causing constipation, it’s essential to consult your healthcare provider for possible alternatives or adjustments.
- Ignoring the Urge to Defecate:
- Ignoring the urge to have a bowel movement can lead to constipation over time.
- When you ignore the urge, the stool can become harder and more difficult to pass.
- It’s important to listen to your body’s signals and respond promptly when you feel the urge to have a bowel movement.
- Neurological Conditions:
- Neurological disorders such as multiple sclerosis, Parkinson’s disease, and spinal cord injuries can affect the nerves that control bowel function.
- This can lead to constipation due to impaired communication between the brain and the intestines.
- Psychological Factors:
- Stress, anxiety, and depression can all affect bowel function.
- The brain and the gut are closely connected, and emotional distress can manifest physically in the form of constipation or other digestive issues.
- Structural Abnormalities:
- Structural abnormalities in the colon or rectum, such as strictures, tumors, or pelvic floor dysfunction, can obstruct the normal passage of stool and lead to constipation.
Clinical Considerations and Management Strategies:
Clinicians evaluating constipation must adopt a comprehensive approach, taking into account the interaction of various factors. Thorough history-taking, physical examination, and diagnostic tests help identify potential contributors, including endocrine disorders. Nevertheless, a holistic assessment should encompass dietary patterns, hydration status, activity levels, medication use, and psychological well-being.
Effective management of constipation requires addressing both underlying conditions and modifiable risk factors. Treatment plans may include targeted therapies for endocrine disorders, such as hormone replacement for hypothyroidism or glycemic control for diabetes. However, lifestyle modifications remain fundamental interventions, including dietary fiber supplementation, adequate hydration, regular exercise, and stress management techniques.
Conclusion:
Constipation complexity reflects a multifaceted interplay involving numerous contributors, including endocrine health conditions. While disorders like hypothyroidism or diabetes can impact bowel function, they seldom act alone.
Instead, constipation often stems from a combination of factors, necessitating a comprehensive approach to diagnosis and management. Clinicians must consider the broader context of an individual’s health, addressing both endocrine disorders and modifiable lifestyle factors to optimize constipation management outcomes.