Introduction to Gut-Brain Connection
Have you ever had a “gut feeling” about something? It turns out that your gut and brain are more connected than you might think. The relationship between gut health and mental health has become a hot topic in medical research, shedding light on how these two seemingly separate parts of the body influence each other. This intricate connection is often referred to as the gut-brain axis, a bidirectional communication system that highlights the profound impact of gut health on our emotions, thoughts, and overall mental well-being.
Table of Contents
What is Gut Health?

Gut health refers to the balance and functionality of the gastrointestinal tract, including the stomach and intestines. When your gut is healthy, it helps digest food, absorb nutrients, and eliminate waste efficiently. But its role extends far beyond digestion—it influences the immune system, hormone regulation, and, importantly, the brain.
The Gut-Brain Axis Explained
The gut-brain axis (GBA) is the two-way communication system between your central nervous system (the brain and spinal cord) and the enteric nervous system (the gut’s “mini-brain”). This connection is mediated by nerves, hormones, and biochemicals like neurotransmitters, making it a crucial player in regulating mood, cognition, and even behavior.
The Science Behind the Gut-Brain Axis
How the Gut Talks to the Brain
The gut and brain communicate constantly via neural, hormonal, and immune pathways. Signals from the gut can influence brain activity, while the brain can affect gut function, often leading to noticeable physical symptoms like butterflies in your stomach during stressful situations.
Key Players: The Vagus Nerve and Neurotransmitters
The vagus nerve acts as a highway, transmitting messages between the brain and the gut. Neurotransmitters like serotonin, dopamine, and gamma-aminobutyric acid (GABA), many of which are produced in the gut, directly impact mood and mental health.
Serotonin’s Role in the Gut
Did you know that nearly 90% of serotonin, a neurotransmitter known for regulating mood, is produced in the gut? This production links gut health directly to emotional stability, sleep patterns, and overall happiness.
Microbiome and Mental Health
What is the Gut Microbiome?
Your gut is home to trillions of microorganisms, including bacteria, viruses, and fungi, collectively known as the microbiome. These tiny organisms play a massive role in digestion, immune defense, and even the production of mood-related chemicals.
When the Microbiome Falls Out of Balance
An imbalanced microbiome, often caused by poor diet, stress, or antibiotics, can lead to dysbiosis—a condition where harmful bacteria outnumber beneficial ones. Dysbiosis has been linked to conditions like depression, anxiety, and brain fog.
Mental Health Conditions Tied to Gut Health
- Depression: Studies show that people with depression often have less diverse gut bacteria.
- Anxiety: Gut inflammation can lead to heightened stress responses.
- Autism Spectrum Disorders: Research suggests a link between gut health and behavioral symptoms in autism.
Role of Diet in Gut and Mental Health
Foods for a Healthy Gut
What you eat directly affects your gut’s microbial balance. A diet rich in fiber, fermented foods (like yogurt and kimchi), and omega-3 fatty acids can foster a healthy microbiome.
Foods to Avoid
Processed foods, high-sugar diets, and excessive alcohol can disrupt gut bacteria, leading to inflammation and poor mental health outcomes.
Probiotics and Prebiotics: The Unsung Heroes
Probiotics are live bacteria that provide health benefits, while prebiotics are the fibers that feed them. Together, they can improve gut health and, by extension, mental health.
Stress and Its Impact on Gut Health
The Vicious Cycle of Stress and Gut Health
Stress doesn’t just affect your mind—it wreaks havoc on your gut. Chronic stress can weaken the gut lining, reduce beneficial bacteria, and trigger inflammation, creating a feedback loop that amplifies mental health struggles.
Chronic Stress and Mental Health
Over time, chronic stress can lead to conditions like irritable bowel syndrome (IBS) and exacerbate symptoms of anxiety and depression.
How to Break the Cycle
- Practice mindfulness techniques like meditation.
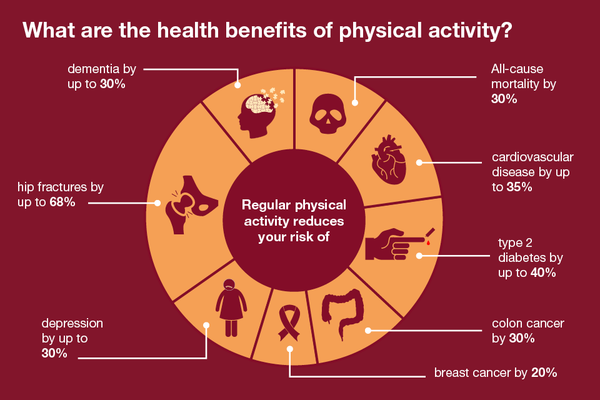
- Incorporate physical activity into your daily routine.
- Ensure adequate rest to allow your body and mind to reset.
The Emerging Field of Psychobiotics
What are Psychobiotics?
Psychobiotics are a groundbreaking category of probiotics specifically designed to impact mental health by improving gut health. Coined in 2013, the term refers to live bacteria that, when consumed in adequate amounts, confer mental health benefits through their interactions with the gut-brain axis. These specialized probiotics work by modulating the gut microbiome, influencing the production of mood-regulating neurotransmitters like serotonin, dopamine, and GABA.
Psychobiotics are found naturally in fermented foods like yogurt, sauerkraut, and kefir, as well as in supplement form. By fostering a healthier gut environment, they can help reduce inflammation, support brain function, and alleviate symptoms of mental health disorders, making them a promising addition to the mental health toolkit.
Evidence Supporting Psychobiotics in Mental Health Treatment

Emerging research strongly supports the efficacy of psychobiotics in mental health care. Clinical trials have shown that specific strains of probiotics, such as Lactobacillus and Bifidobacterium, can reduce symptoms of anxiety and depression. These strains influence the gut microbiome, lowering inflammation and supporting the production of calming neurotransmitters.
In one study, participants with mild to moderate depression experienced significant mood improvements after taking a psychobiotic supplement for eight weeks. Other research suggests psychobiotics can enhance cognitive function, memory, and stress resilience, particularly in populations dealing with chronic stress or neurodegenerative diseases.
Although still in its infancy, the field of psychobiotics offers hope for treating mental health conditions without the side effects often associated with pharmaceuticals.
Future Potential of Psychobiotics in Medicine
The future of psychobiotics is incredibly promising. As research advances, we may see personalized psychobiotic treatments tailored to an individual’s unique gut microbiome. This customization could revolutionize mental health care by addressing root causes rather than just managing symptoms.
Psychobiotics may also play a preventive role, helping individuals maintain mental health before issues arise. Additionally, combining psychobiotics with traditional therapies, such as cognitive-behavioral therapy (CBT) or medication, could enhance treatment outcomes for conditions like anxiety, depression, and even PTSD.
Despite these prospects, more large-scale studies are needed to fully understand psychobiotics’ mechanisms and establish guidelines for their use in mainstream medicine.
Practical Tips to Enhance Gut and Mental Health

Building a Gut-Friendly Lifestyle
Enhancing gut health begins with lifestyle choices. A balanced diet, hydration, stress management, and regular exercise are cornerstones of a gut-friendly lifestyle.
- Eat whole foods: Focus on fruits, vegetables, whole grains, and lean proteins.
- Incorporate fermented foods: Yogurt, kimchi, and kombucha can introduce beneficial bacteria to your gut.
- Limit processed foods: Avoid excessive sugar, unhealthy fats, and additives that harm the microbiome.
Lifestyle changes don’t need to be overwhelming—small, consistent steps can lead to significant improvements over time.
Exercise and Its Dual Benefits on Gut and Mental Health
Physical activity benefits both your gut and your brain. Regular exercise promotes a diverse microbiome, which in turn influences neurotransmitter production and reduces inflammation. From walking to high-intensity workouts, exercise has been shown to improve mood, reduce anxiety, and support cognitive function.
Additionally, exercising stimulates the release of endorphins, the body’s “feel-good” chemicals, while also increasing gut motility, aiding digestion, and preventing disorders like constipation and bloating.
Sleep’s Role in Maintaining Balance
Sleep is a crucial yet often overlooked factor in gut and mental health. Poor sleep disrupts the gut microbiome, which can lead to mood disorders. Conversely, gut imbalances can disturb sleep patterns, creating a vicious cycle. Aim for 7–9 hours of quality sleep each night to give your gut and brain time to repair and rejuvenate.
Some tips for better sleep include:
- Maintaining a consistent sleep schedule.
- Limiting caffeine and heavy meals close to bedtime.
- Creating a calming pre-sleep routine, such as reading or meditating.
Medical Insights and When to Seek Help
Signs of Poor Gut Health Affecting Mental Health
Recognizing when gut health might be impacting mental health is key. Symptoms to watch for include:
- Persistent digestive issues, such as bloating, constipation, or diarrhea.
- Chronic fatigue or low energy levels.
- Frequent mood swings, anxiety, or depressive symptoms.
- Poor concentration or brain fog.
If these symptoms persist despite lifestyle changes, it’s essential to seek professional help.
Consulting Professionals: Gastroenterologists and Psychiatrists
Both gastroenterologists and psychiatrists play vital roles in managing the gut-brain connection. A gastroenterologist can help identify gut-related disorders like IBS or dysbiosis, while a psychiatrist can address the mental health implications.
In some cases, an integrative approach involving both specialists may be the most effective. Personalized treatment plans might include dietary adjustments, probiotic supplementation, therapy, or medication.
Conclusion
The intricate relationship between gut health and mental health underscores the importance of a holistic approach to well-being. The gut-brain axis serves as a powerful reminder that the body and mind are deeply interconnected, and nurturing one can profoundly influence the other.
Improving your gut health doesn’t have to be complicated. With mindful eating, regular exercise, stress management, and adequate sleep, you can foster a thriving gut microbiome that supports mental clarity, emotional resilience, and overall happiness. The key is to start small, stay consistent, and seek professional guidance when needed.
Frequently Asked Questions
1. How does gut health influence emotions?
Gut health affects emotions through the gut-brain axis, where neurotransmitters like serotonin and GABA, produced in the gut, regulate mood and stress responses.
2. Can improving gut health reduce anxiety?
Yes, improving gut health through diet, probiotics, and stress management can lower anxiety levels by enhancing the gut microbiome and reducing inflammation.
3. What foods are best for gut-brain health?
Foods rich in fiber (like fruits and vegetables), fermented foods (yogurt, kefir), and omega-3 fatty acids are excellent for gut-brain health.
4. Are probiotics safe for everyone?
Most people can safely consume probiotics, but individuals with weakened immune systems or underlying health conditions should consult a doctor first.
5. How long does it take to see improvements in mental health by improving gut health?
Changes in mental health from improved gut health can take a few weeks to months, depending on individual factors like diet, lifestyle, and baseline gut health.