Unlock the secrets to overcoming plantar fasciitis with our guide on natural remedies. Dive into a world of effective, non-invasive solutions for lasting foot pain relief and improved mobility. Start your journey to recovery today!

Introduction
Plantar fasciitis is a term that has become increasingly familiar to many, especially among runners, athletes, and those leading active lifestyles. However, the condition extends beyond the realm of sports, affecting a broad demographic. Characterized by sharp, stabbing pain in the bottom of the foot, plantar fasciitis can turn simple activities like walking or standing into daunting tasks. This article aims to unravel the mysteries of plantar fasciitis, shedding light on its root causes and symptoms, to provide a clearer understanding and pave the way for effective management.
Table of Contents
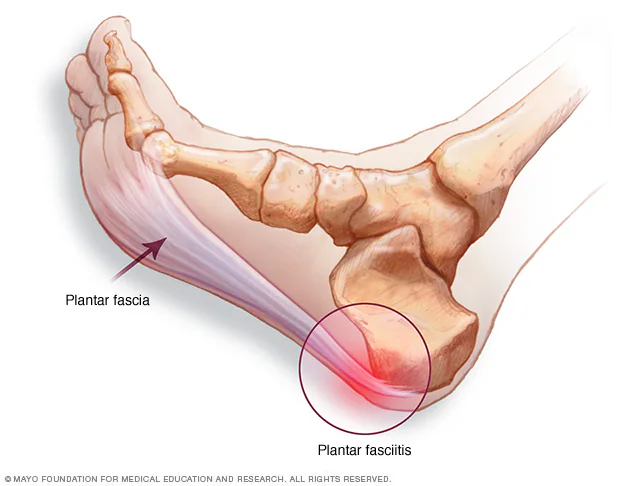
What is Plantar Fasciitis?
Plantar fasciitis is an inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. It acts like a shock-absorbing bowstring, supporting the arch in your foot. When tension and stress on this bowstring become too great, small tears can arise in the fascia. Repeated stretching and tearing can cause the fascia to become irritated or inflamed.
Root Causes of Plantar Fasciitis

Understanding the causes of plantar fasciitis is crucial for prevention and treatment. The condition does not discriminate by age or fitness level, though certain factors can increase your risk:
| Excessive Load on the Foot |
| Activities that place a lot of stress on your heel and attached tissue — such as long-distance running, ballet dancing, and aerobic dance — can contribute to the onset of plantar fasciitis. |
| Foot Structure |
| People with flat feet, a high arch, or even an abnormal pattern of walking can put extra stress on the plantar fascia. |
| Improper Footwear |
| Wearing shoes that are worn out, lack support, or are not suited for your activity level can increase your risk. |
| Occupation |
| Jobs that require you to be on your feet for extended periods, especially on hard surfaces, can contribute to the condition. |
| Weight |
| Excess body weight can put extra stress on the plantar fascia, making obesity a significant risk factor. |
Symptoms of Plantar Fasciitis

The symptoms of plantar fasciitis are distinct and primarily centered around pain in the foot:
| Sharp Pain in the Heel |
| The most common symptom is a sharp, stabbing pain in the inside part of the bottom of your heel. This pain is usually the worst with the first few steps after waking up, although it can also be triggered by long periods of standing or when you stand up after sitting. |
| Pain After Exercise |
| Interestingly, the pain isn’t typically felt during exercise but rather just after stopping. |
| Stiffness and Tenderness |
| The bottom of the foot may feel stiff or tender to the touch, especially in the morning or after periods of inactivity. |
Comprehensive Treatment Options for Plantar Fasciitis

Conservative Treatments (Lifestyle and Home Remedies)
Rest Periods
The plantar fascia is subjected to continuous stress throughout the day, especially for individuals with active lifestyles or those whose jobs require extended periods of standing. Introducing regular rest periods allows the inflamed tissue to recover, reducing the cycle of stress and inflammation. Elevating your feet above heart level during these breaks can further aid in reducing swelling by improving circulation.
Apply Ice Regularly
Ice therapy works by constricting blood vessels, which can decrease inflammation and numb the surrounding area, providing immediate pain relief. For an effective massage, roll a frozen water bottle under your foot, focusing on the arch and heel area. This method not only reduces inflammation but also provides a gentle stretch to the plantar fascia.
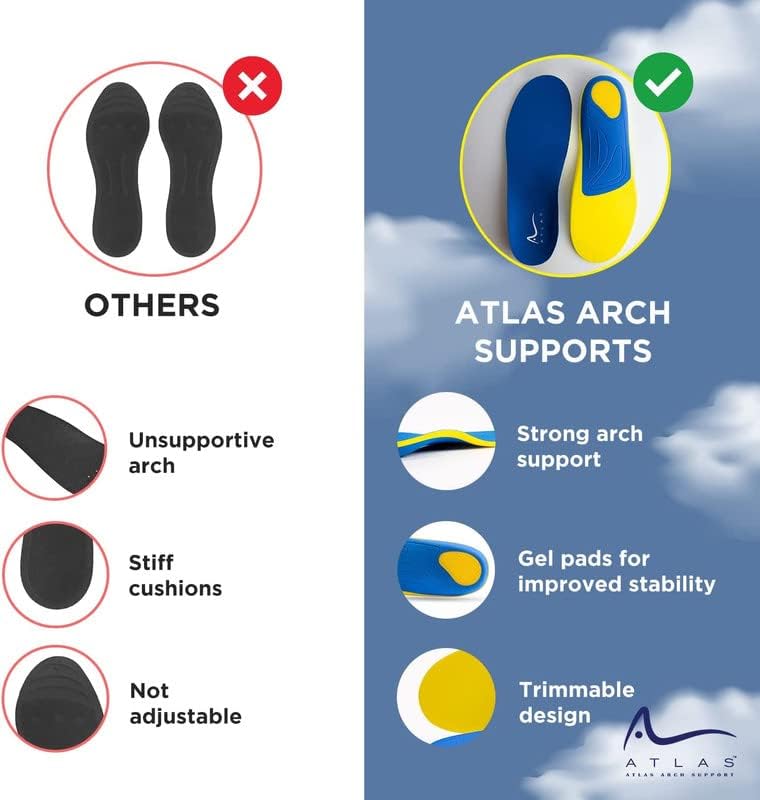
Orthotic Inserts
Orthotic inserts play a crucial role in redistributing foot pressure, supporting the arch, and cushioning the heel. By aligning the foot properly, orthotics can prevent abnormal stretching of the plantar fascia. Both over-the-counter and custom-fitted orthotics can be beneficial, depending on the individual’s specific foot structure and the severity of symptoms.
Start Your Day with Gentle Stretches
Morning pain associated with plantar fasciitis is often due to the foot being in a relaxed position overnight, leading to tightening of the plantar fascia. Gentle stretching exercises in the morning can increase flexibility and decrease pain by warming up the tissue before weight-bearing activities. The towel stretch is particularly effective as it mimics the natural flex and extension of the foot, similar to walking, but without the stress.
Physical Therapy
Physical therapy for plantar fasciitis focuses on strengthening and stretching exercises that target the foot, ankle, and calf muscles. Strengthening these areas can improve foot mechanics and reduce the strain on the plantar fascia. A physical therapist may also use modalities such as ultrasound therapy or taping to support the foot and alleviate pain.
Weight Management
Excess body weight increases the load on the plantar fascia with every step taken, exacerbating the pain and inflammation. Achieving and maintaining a healthy weight through a balanced diet and regular exercise can significantly reduce the pressure on your feet and alleviate symptoms of plantar fasciitis.
Supportive Shoes
Footwear that provides adequate arch support and cushioning can absorb shock and reduce stress on the plantar fascia. Shoes should also have a firm heel counter to stabilize the heel and a flexible sole to allow for natural foot movement. Replacing worn-out shoes regularly is crucial to ensure ongoing support and cushioning.
Exercise Smart
Engaging in low-impact exercises minimizes stress on the plantar fascia while allowing individuals to stay active. Activities like swimming and cycling maintain cardiovascular fitness without placing additional strain on the feet. For those who prefer running, switching to soft surfaces and gradually increasing intensity can help minimize the risk of aggravating plantar fasciitis.
Medications
1. Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs), such as ibuprofen and naproxen, can help reduce pain and inflammation associated with plantar fasciitis.
Advanced Treatments
1. Corticosteroid Injections: For more severe cases, corticosteroid injections directly into the affected area can provide temporary relief from pain and inflammation. However, these are typically used sparingly due to potential side effects.
2. Extracorporeal Shock Wave Therapy (ESWT): ESWT can be an option when other treatments have failed. It uses sound waves to stimulate healing within the plantar fascia, promoting tissue repair and pain relief.
3. Platelet-Rich Plasma (PRP) Injections: PRP involves injecting a concentration of the patient’s own platelets into the affected area to promote healing of the injured tendons, ligaments, muscles, and joints.
Surgical Options
When conservative treatments for plantar fasciitis do not result in significant improvement, and the patient continues to experience debilitating pain, surgical options may be considered. These procedures are typically reserved for cases where persistent pain affects the quality of life and all non-surgical interventions have been exhausted. Here’s a more detailed look at the common surgical procedures for plantar fasciitis:
1. Plantar Fascia Release
Procedure: Plantar fascia release surgery is performed to cut through part of the plantar fascia ligament, thereby releasing tension and reducing inflammation. This procedure can be done through open surgery or more commonly through endoscopic surgery, which is minimally invasive. The latter involves making small incisions near the heel, and using a tiny camera (endoscope) to guide the surgery, which cuts only a portion of the plantar fascia. This method typically results in shorter recovery times and less post-operative pain compared to open surgery.
Recovery and Outcomes: Recovery from plantar fascia release surgery varies, with many patients able to walk shortly after the procedure using a boot or cast to protect the foot. Complete recovery and return to full activities can take several weeks to months. While many patients experience significant relief from pain, as with any surgery, there are risks including incomplete relief of pain, development of new foot problems, or nerve damage.


2. Gastrocnemius Recession
Procedure: Gastrocnemius recession is aimed at lengthening the calf muscles (specifically the gastrocnemius muscle). Tight calf muscles can contribute to excessive strain on the plantar fascia. This procedure involves making an incision behind the knee or at the calf, and then lengthening the muscle by cutting and repositioning it. This reduces the stress on the plantar fascia and can alleviate pain. Gastrocnemius recession is often considered when patients have difficulty flexing their feet despite prolonged stretching.
Recovery and Outcomes: The recovery process for gastrocnemius recession involves several weeks of wearing a boot or cast to immobilize the foot and allow the muscle to heal in its new lengthened position. Physical therapy is typically required to regain strength and flexibility in the calf muscle. Most patients report relief from plantar fasciitis symptoms and improved flexibility in the foot and ankle. However, potential risks include reduced calf strength or complications from surgery.
Making the Decision for Surgery
Deciding to proceed with surgery for plantar fasciitis involves careful consideration of the potential benefits and risks. It’s important to have a thorough discussion with a healthcare provider, ideally a specialist in foot and ankle surgery, to understand the expected outcomes, recovery process, and how surgery fits into your overall treatment plan. Surgery should be seen as a partnership between you and your surgeon, with a clear understanding of the goals and a realistic expectation of the results.
FAQ Section

Q1: What exactly is plantar fasciitis?
A1: Plantar fasciitis is an inflammation of the plantar fascia, a thick band of tissue that runs across the bottom of your foot, connecting your heel bone to your toes. It’s often characterized by sharp, stabbing pain in the heel or bottom of the foot.
Q2: What causes plantar fasciitis?
A2: The condition can arise from excessive load on the foot, improper footwear, certain physical activities, and even from an individual’s foot structure. Obesity can also increase the risk due to the extra stress on the plantar fascia.
Q3: How can I relieve plantar fasciitis pain at home?
A3: Effective home remedies include regular rest periods, applying ice, using orthotic inserts, engaging in gentle stretches, and wearing supportive shoes. These strategies can significantly alleviate pain and promote healing.
Q4: Are there any advanced treatments for severe cases?
A4: Yes, for more persistent cases, options like corticosteroid injections, extracorporeal shock wave therapy (ESWT), and platelet-rich plasma (PRP) injections may be considered. These treatments aim to reduce inflammation and stimulate healing.
Conclusion
Living with plantar fasciitis doesn’t have to be a life sentence of pain and discomfort. By embracing natural remedies and making informed choices about your foot health, you can navigate your way to relief and recovery. Remember, every step towards understanding and treating plantar fasciitis is a step towards reclaiming your mobility and quality of life. Don’t let foot pain hold you back—take control and stride into a pain-free future.