Dive into our comprehensive guide on Shin Splints, offering groundbreaking strategies for prevention, diagnosis, and treatment. Empower yourself with expert advice to conquer this common yet debilitating condition and stride towards a pain-free life.

Introduction
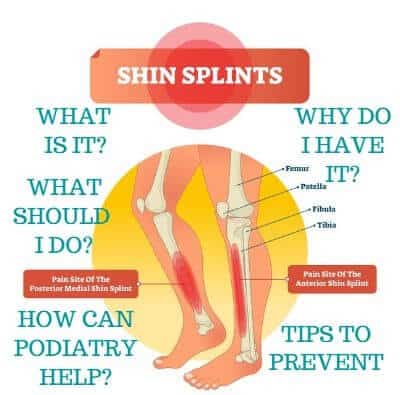
Shin splints, a term familiar yet dreaded by athletes and fitness enthusiasts alike, refer to the agonizing pain along the shinbone, a plight signaling overuse and stress in this critical area. This guide peels back the layers of shin splints, providing a deep dive into their causes, symptoms, and, most importantly, the pathways to relief. Whether you’re a seasoned marathoner or a weekend warrior, understanding shin splints is the first step toward reclaiming your stride and enjoying your activities pain-free.
Table of Contents
Causes of Shin Splints
Shin splints are a common affliction, particularly among athletes and those engaged in high-impact activities, resulting from excessive strain on the shinbone (tibia) and its surrounding tissues. Here’s a closer look at the primary factors contributing to this painful condition:
1. Overuse in Physical Activities
The leading cause of shin splints is the overexertion of leg muscles, tendons, and bone tissue. This condition is prevalent in individuals participating in activities that demand extensive leg work, such as running, dancing, and military exercises. The repetitive nature of these activities, especially without adequate rest, places significant stress on the lower legs, triggering shin splints. The risk increases with abrupt enhancements in activity intensity or duration, surpassing the body’s capacity to adjust.
2. Improper Footwear
The choice of footwear is critical in providing the necessary support and cushioning for the feet during physical exertions. Inadequate shoes, lacking in proper support or not tailored for the activity at hand, can greatly increase the risk of shin splints. Footwear that fails to offer enough impact absorption or does not address biomechanical foot imbalances can lead to an uneven distribution of force, thereby straining the shinbone and its adjacent tissues.

3. Biomechanical Imbalances
An individual’s foot and leg structure significantly affects their susceptibility to shin splints. Biomechanical issues, such as flat feet (overpronation) or high arches (supination), can cause an uneven weight and stress distribution across the leg, adding extra pressure on the shinbone. Additionally, incorrect techniques in running, jumping, or walking can intensify the risk by placing unusual stress on the lower leg, disrupting the leg’s natural alignment and function.
4. Muscular Imbalances and Flexibility Issues
Shin splints can also stem from muscular imbalances and insufficient flexibility in the lower leg. Tight calf muscles, weak ankles, and poor flexibility can lead to altered gait and running patterns, increasing the shinbone’s stress. Engaging in regular stretching and strengthening exercises for the lower leg muscles can help alleviate these issues by enhancing muscle balance and flexibility.
5. Surface and Environmental Factors
Performing activities on hard or uneven terrains can further heighten the risk of shin splints due to the increased impact forces on the shinbone. Likewise, training under adverse environmental conditions without adjusting the equipment or activity intensity can also amplify the stress on the lower legs.
Symptoms
Shin splints manifest primarily as pain along the inner side of the shinbone, among other symptoms:
Pain Along the Inner Edge of the Shinbone
The defining feature of shin splints is a distinct pain felt along the tibia’s inner edge. This pain, which can be sharp, aching, or throbbing, signals stress and inflammation in the tissues connecting muscles to the bone.
Increased Sensitivity
The area affected by shin splints often becomes particularly sensitive to touch, displaying tenderness and soreness. The severity of this soreness can range from a mild annoyance to intense pain that interferes with daily tasks.
Swelling and Inflammation
Stress on the shinbone and its adjacent tissues can lead to visible swelling and signs of inflammation. Although usually mild, this swelling adds to the overall discomfort and serves as a measure of the condition’s intensity.
Pain During Activity
A common complaint is a dull or throbbing pain that grows more intense during physical activities, such as running or jumping. This pain may start only at the beginning of an activity but can persist or worsen as the shin splints progress.
Increased Pain with Pressure or Impact
The pain from shin splints is notably worse when pressure is applied to the shinbone or during impact-heavy activities. This is especially evident when pressing directly on the shin or while walking or running on hard surfaces.
Additional Symptoms
Some individuals might also experience stiffness in the muscles and a limited range of motion in the affected leg. Additionally, the pain can spread to nearby areas, leading to a generalized discomfort in the lower leg.
Progression of Symptoms
Initially, symptoms of shin splints may only appear during or right after exercise. However, without appropriate care and rest, these symptoms can evolve to a point where pain is constant, even at rest, severely impacting mobility and quality of life.
Diagnosis
Diagnosing shin splints involves a thorough evaluation to accurately pinpoint the condition and differentiate it from other causes of lower leg pain. This comprehensive approach helps tailor the treatment effectively. Here’s a breakdown of the diagnostic steps for shin splints:
Review of Medical History
Initial Consultation: The process starts with a detailed review of the patient’s medical history, including any past leg injuries or conditions that might affect the lower legs. Discussions also encompass the patient’s exercise habits, any recent uptick in physical activity, and previous leg pain treatments.
Symptom Assessment: A critical part of the diagnosis is understanding the symptoms’ specifics, such as when the pain started, its persistence, and activities that worsen or relieve the pain. This information is key to distinguishing shin splints from other similar conditions.
Physical Examination
Observation and Palpation: The doctor will examine the leg for swelling, redness, or deformities. By palpating, or feeling, the shin area, the doctor can identify tender spots along the shinbone, a hallmark of shin splints.
Functional Testing: The patient may be asked to perform simple movements or exercises. This helps assess the leg’s biomechanics, muscle strength, and flexibility, and pinpoint what triggers the pain, such as specific walking patterns or jumping.
Advanced Imaging Tests
If necessary, further tests may be conducted to exclude other conditions:
X-rays: While shin splints won’t appear on X-rays, this test can eliminate the possibility of bone fractures that mimic shin splint symptoms.
MRI Scans: For a closer look at the soft tissues around the shinbone, MRI scans can be invaluable. They can detect bone stress reactions or differentiate shin splints from injuries to muscles or connective tissues.
Bone Scans: To investigate potential stress fractures, a bone scan may be performed. This involves a minor radioactive material injection, highlighting bone remodeling areas, indicative of fractures or significant stress.
Differential Diagnosis
A vital step in diagnosing shin splints is ruling out conditions with similar symptoms, such as compartment syndrome, stress fractures, and muscle strains. This ensures the treatment plan specifically targets shin splints, addressing the correct underlying issue.
Treatment
Treating shin splints involves a multifaceted approach tailored to the severity and root causes of the condition. Here’s a comprehensive guide to managing and eventually overcoming shin splints:
1. Rest and Recovery
Key to Recovery: Taking a break from activities that aggravate shin splints is crucial. This rest period allows the inflamed tissues around the shinbone to recover. Depending on the shin splints’ severity, this may require temporarily stopping certain exercises or adjusting overall activity levels to minimize leg strain.
Careful Activity Resumption: As symptoms improve, a cautious and gradual reintroduction to physical activities is advised, with a mindful approach to controlling intensity and duration to avoid relapse.
2. Ice Therapy
Managing Pain and Swelling: Applying ice packs to the shin area for 20-30 minutes multiple times daily can effectively reduce inflammation and alleviate pain. This method helps narrow blood vessels, lessening swelling and providing relief.

3. Compression Techniques
Enhanced Support: Utilizing compression sleeves or wraps around the lower leg can aid in reducing swelling and offer additional support. These devices gently compress the area, boosting circulation and aiding recovery.
4. Medication for Symptom Relief
Anti-Inflammatory Medications: NSAIDs, like ibuprofen or naproxen, are often recommended for their pain-relieving and anti-inflammatory properties. It’s important to follow healthcare guidance when using these medications to minimize side effects.

5. Physical Therapy and Exercises
Rehabilitation and Prevention: Physical therapy is a cornerstone in treating shin splints, offering customized stretching and strengthening exercises to bolster the muscles around the shin. This not only aids in recovery but also equips patients with preventive techniques to avoid future issues.
6. Orthotic Support
Biomechanical Support: For those with underlying foot structure issues, such as overpronation or high arches, custom orthotics can offer necessary support and cushioning. These devices help evenly distribute weight across the foot, easing the burden on the shinbone and adjacent tissues.

Incorporating these strategies can significantly alleviate shin splint symptoms, paving the way for a full return to activities with an informed approach to prevention and care.
Prevention
To ward off shin splints, especially for athletes and active individuals, adopting preventive strategies is essential:
1. Progressive Training Adaptation
Smart Progression: Slowly ramping up the intensity and volume of physical activities allows the lower legs to adapt without being overwhelmed, minimizing the risk of shin splints.
Rest Integration: Including rest days in your routine is vital for recovery, helping to prevent undue stress on the shinbone and surrounding tissues.
2. Optimal Footwear Selection
Choosing the Right Shoes: Selecting shoes with adequate support and cushioning, specific to your activity, plays a significant role in shin splint prevention. Regularly updating footwear ensures ongoing protection and impact absorption.
Expert Fitting: Seeking professional advice for shoe fitting can further tailor your choice to your foot type and walking or running style, enhancing prevention efforts.
3. Varied Exercise Routines
Balanced Activity: Mixing different types of exercises helps evenly distribute physical stress, combining high-impact activities with lower-impact exercises to safeguard against overuse.
4. Effective Warm-up and Cool-down Routines
Pre-Activity Preparation: Beginning workouts with dynamic stretching warms up the body, enhancing muscle flexibility and blood flow, reducing injury risks.
Post-Activity Recovery: Ending sessions with static stretching aids in muscle relaxation and flexibility, contributing to shin splint prevention.
5. Targeted Strengthening and Flexibility Exercises
Strengthening Key Muscles: Exercises aimed at fortifying the muscles around the shinbone enhance leg stability and support, diminishing stress on the shin.
Improving Flexibility: Regularly stretching the lower leg muscles maintains proper motion range, preventing the tightness that can lead to shin splints.
FAQ Section
Q: What exactly are shin splints? A: Shin splints describe pain along the inner edge of the shinbone, resulting from stress on the bone and surrounding tissues, often due to overuse in physical activities.
Q: What causes shin splints? A: Key contributors include overuse in physical activities, inadequate footwear, biomechanical imbalances, muscular and flexibility issues, and harsh training surfaces or environments.
Q: How can I tell if I have shin splints? A: Symptoms include sharp, aching pain along the shinbone, increased sensitivity, swelling, pain that intensifies during physical activity, and discomfort when pressure is applied.
Q: What are the best treatment options for shin splints? A: Effective treatments encompass rest and recovery, ice therapy, compression techniques, medication for symptom relief, physical therapy, and orthotic support for those with foot structure issues.
Q: Can shin splints be prevented? A: Yes, through progressive training adaptation, selecting the right footwear, incorporating varied exercise routines, and following effective warm-up and cool-down routines.
Conclusion
Shin splints, while challenging, are not insurmountable. Armed with the right knowledge and strategies, you can navigate through this condition with confidence. Embracing a holistic approach that includes understanding the causes, recognizing symptoms early, and applying targeted treatments and preventive measures, you can not only alleviate shin splints but also enhance your overall athletic performance and well-being. Remember, listening to your body and responding with care is paramount. With patience and persistence, you can overcome shin splints and return to your favorite activities with vigor and vitality.