Heel pain is a common foot condition that can be caused by a variety of factors, ranging from mechanical issues to systemic diseases. Understanding the risk factors for heel pain is crucial for both prevention and effective management. Here’s a detailed look at the causes of heel pain and the risk factors associated with it.

Table of Contents
Causes of Heel Pain
The causes of heel pain you’ve listed cover a range of conditions affecting different structures within the foot. Here’s a more detailed look at each cause to help understand how they lead to heel pain:
- Plantar Fasciitis: The plantar fascia is a thick band of tissue that runs along the bottom of your foot, connecting the heel to the front of your foot. Plantar fasciitis occurs when this band becomes inflamed, leading to sharp pain in the heel, especially with the first steps in the morning or after periods of rest. Overuse, excessive weight, or unsupportive footwear can strain the plantar fascia, leading to this condition.
- Achilles Tendinitis: This condition involves inflammation of the Achilles tendon, which is the large tendon that connects the calf muscles to the heel bone. It’s often the result of repetitive stress to the tendon, not allowing enough time for recovery between activities. Symptoms include pain and stiffness along the Achilles tendon, particularly in the morning, which improves with mild activity.
- Heel Bursitis: Bursitis of the heel occurs when the bursa, a fluid-filled sac located at the back of the heel, becomes inflamed. This condition can cause deep pain at the back of the heel, which may worsen with activity. It can be caused by wearing shoes that rub or press against the back of the heel, excessive walking or running, or an injury to the heel.
- Heel Spurs: Heel spurs are bone growths that develop on the underside of the heel bone. They often form where the plantar fascia tissue band connects to the heel bone. While heel spurs themselves may not cause pain, they are commonly associated with plantar fasciitis, leading to similar symptoms.
- Tarsal Tunnel Syndrome: This syndrome is similar to carpal tunnel syndrome in the wrist but occurs in the foot. It’s caused by compression of the posterior tibia nerve, which runs along the inside of the ankle and the foot. Symptoms include pain, tingling, or numbness in the heel, which may extend to the sole of the foot.
- Stress Fractures: Stress fractures in the heel are tiny cracks in the bone, usually caused by repetitive force, often from overuse, such as with running or jumping. They can also arise from normal use of a bone that’s weakened by a condition such as osteoporosis. Stress fractures cause localized pain that can worsen with weight-bearing activity.
- Fat Pad Atrophy: The heel has a natural fat pad that provides cushioning and support during walking and other activities. Over time or due to certain medical conditions, this fat pad can wear away or thin out, leading to decreased cushioning beneath the heel. This condition results in increased pressure and pain when standing or walking.
Addressing heel pain effectively requires identifying the underlying cause. Treatments may include rest, ice, physical therapy, orthotic devices, medication, or surgery in severe cases. It’s crucial for individuals experiencing heel pain to seek medical advice for a proper diagnosis and treatment plan.
Risk Factors for Heel Pain
The risk factors for heel pain you’ve listed highlight how a combination of lifestyle, physical conditions, and medical issues can contribute to the development of this condition. Understanding these risk factors can help in preventing heel pain or managing it more effectively if it occurs. Here’s a closer examination of each factor:

- Age: As individuals age, the structures of the foot can wear down over time. The fat pad on the heel thins, and the plantar fascia can lose its elasticity, leading to increased risk of injury and pain. Middle-aged and older adults often experience these changes, making them more susceptible to heel pain.
- Obesity: Carrying excess body weight significantly increases the stress on the feet, particularly the heel. This additional pressure can lead to or exacerbate conditions like plantar fasciitis and heel spurs, making obesity a prominent risk factor for heel pain.
- Exercise: High-impact activities, such as long-distance running, ballet dancing, and aerobic dance, exert considerable stress on the foot and heel. Without adequate rest and proper technique, this stress can lead to overuse injuries, including those that cause heel pain.
- Foot Mechanics: The structure and mechanics of the foot play a crucial role in distributing body weight during movement. Flat feet (overpronation) and high arches (underpronation) can both lead to an uneven distribution of pressure, increasing the risk of heel pain. Similarly, abnormal walking patterns can place additional stress on the heel and attached tissues.
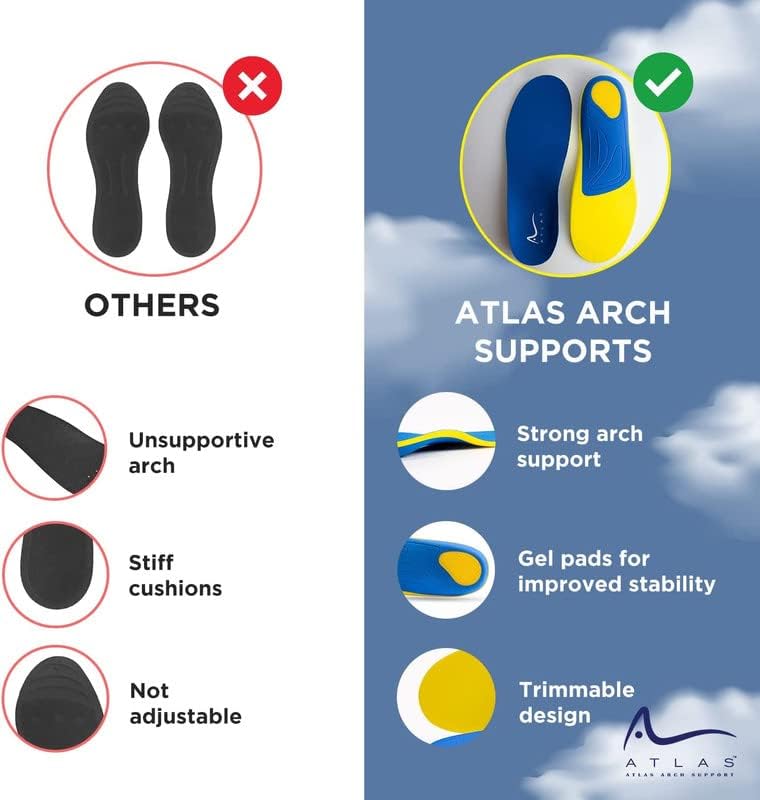
- Improper Footwear: Wearing shoes that lack proper support or cushioning can contribute significantly to the development of heel pain. This includes shoes with hard soles, inadequate arch support, or shoes that do not fit well, all of which can increase the strain on the heel and surrounding structures.
- Occupational Risk Factors: Jobs that involve prolonged standing or walking on hard surfaces can put excessive stress on the feet. Occupations in the healthcare, retail, and manufacturing sectors, for example, can increase the risk of developing heel pain due to the constant pressure and impact on the heel.
- Medical Conditions: Certain systemic diseases, such as rheumatoid arthritis and psoriasis, are associated with inflammation that can affect the feet, including the heel. Fibromyalgia, a condition characterized by widespread pain, can also increase sensitivity to pain in the heel. These medical conditions can exacerbate or directly contribute to the development of heel pain.
Understanding these risk factors is crucial for both prevention and treatment. Preventative measures may include maintaining a healthy weight, choosing appropriate footwear, incorporating foot exercises to improve strength and flexibility, and modifying exercise routines to reduce stress on the heel. For those already experiencing heel pain, addressing these risk factors as part of a comprehensive treatment plan can significantly improve outcomes.
Prevention and Management
Preventing and managing heel pain effectively requires a proactive approach to address the modifiable risk factors and implement strategies that support foot health. Here’s a closer look at prevention and management techniques:

- Maintain a Healthy Weight: Keeping your weight within a healthy range reduces the stress on your feet and heels, decreasing the risk of developing conditions like plantar fasciitis.
- Wear Supportive and Well-Fitting Shoes: Shoes should provide good arch support, a cushioned sole, and enough room to move your toes. Avoid high heels and shoes with inadequate support, especially if you spend a lot of time on your feet.
- Incorporate Foot Exercises: Exercises that strengthen the foot muscles and improve flexibility can help prevent heel pain. Stretching the Achilles tendon and the plantar fascia, as well as strengthening exercises for the foot and lower leg, are particularly beneficial.
- Modify Exercise Routines: If you participate in high-impact sports or activities, consider incorporating low-impact exercises like swimming or cycling into your routine to reduce stress on your heels.
- Gradually Increase Activity Levels: Avoid sudden increases in exercise intensity or duration, which can lead to overuse injuries. Gradually building up allows your body to adapt to new stresses.
Management
For those already experiencing heel pain, a comprehensive treatment plan tailored to the individual’s specific condition is essential:
1. Rest and Ice: Reducing or stopping activities that cause heel pain and applying ice can help reduce inflammation and pain.

2. Anti-inflammatory Medications: Nonsteroidal anti-inflammatory drugs (NSAIDs) can help reduce pain and inflammation. Always use these medications as directed by a healthcare professional.
3. Physical Therapy: A physical therapist can develop a personalized exercise program to stretch and strengthen the foot, ankle, and lower leg muscles, improving foot mechanics and alleviating pain.
4. Orthotic Devices: Custom orthotics or over-the-counter arch supports can provide necessary support to the foot, distributing pressure more evenly and alleviating stress on the heel.
5. Surgery: In severe cases where conservative treatments have not provided relief, surgery may be considered. Surgical options depend on the underlying cause of the heel pain and are usually seen as a last resort.
Professional Consultation
Consulting with a healthcare professional, such as a podiatrist, is crucial for anyone experiencing persistent heel pain. They can offer a diagnosis, recommend appropriate treatment options, and provide guidance on preventive measures to avoid recurrence. Early intervention is key to preventing the condition from worsening and ensuring a quick return to daily activities.
By addressing the risk factors, adopting preventive measures, and seeking appropriate treatment when necessary, individuals can significantly reduce their risk of developing heel pain or manage existing conditions effectively, leading to improved overall foot health and quality of life.